Abstract
Background and aims:
Angioimmunoblastic T cell Lymphoma (AITL) is a subtype of peripheral T cell lymphoma that is generally felt to be aggressive and of poor prognosis. It is characterized as a lymphoma associated with inflammatory and immune conditions, typically seen in the older population and presenting at more advanced stages. The International T-Cell Lymphoma project recently reported a novel AITL score comprising of age, ECOG performance status, serum CRP level and serum B2-microglobulin level; the latter 2 variables suggesting a pro-inflammatory state. They also found that progression of disease within 24 months (POD24) to be strongly prognostic. In our Asian multicenter study, we aim to investigate the clinical prognostic factors affecting the outcomes of our AITL patients and attempt to identify a prognostic index that would be relevant to our Asian population.
Methods:
Patients who were consecutively diagnosed with AITL and seen at National Cancer Centre Singapore and Singapore General Hospital between June 1999 and Dec 2019 were retrospectively analyzed. Relevant demographical and clinical characteristics were collected. Median duration of follow up was 19.7 months. Outcomes of interest were that of 5-year overall survival (OS) and 5-year progression free survival (PFS). POD24 as defined by progression of disease within 24 months was also analyzed for its prognostic significance. Kaplan meier curves were plotted to estimate survival for each individual clinical parameter. Parameters found to be significant on univariate analysis were subsequently used in generation of multivariate cox regression models.
Results:
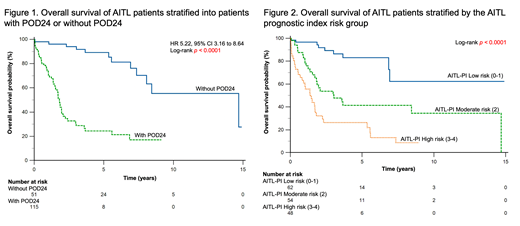
A total of 166 patients were included. The median age was 62.1 years. The majority of our patients (92.8%) had good performance status of ECOG 0-1 and 77.7% presented at advanced stages (Ann Arbor stage 3-4). The median PFS and OS was 1.5 years and 5.5 years respectively. The estimated 5-year PFS and OS was 40% and 53% respectively. Univariate analyses of various parameters were significant for age >60 years, presence of B symptoms, ECOG >1, Ann Arbor stage 3-4, bone marrow involvement, elevated serum lactate dehydrogenase > upper limit normal, elevated total white cell count > 12 x 10 9/L and low platelet count < 150,000/mm 3. In the multivariate analyses, age >60 years, bone marrow involvement, elevated total white cell count and low platelet count were associated with poorer PFS and OS. This allowed for a prognostic index (AITL-PI) differentiating patients into low (0-1 factors, n=62), moderate (2 factors, n=54) and high (3-4 factors, n=48) risk subgroups with 5-year OS of 83%, 41% and 26% respectively. The corresponding 5-year PFS of the low, moderate and high risk subgroups are 69%, 29% and 14%. Likewise, POD24 proved to be strongly prognostic in our cohort as patients with POD24 had a 5-year OS of 24%, whereas those without POD24 had a 5-year OS of 90% (p<0.0001).
Conclusion:
We validated POD24 as a strong prognostic factor. Our AITL-PI was able to identify 3 different subgroups of patients with disparate outcomes based on their presenting clinical parameters. Further work can be done to elucidate if there are unique pathological or molecular characteristics in these individual risk groups that can further guide treatment choices.
No relevant conflicts of interest to declare.